DIAGNOSIS
Diabetes is a chronic, progressive disease that too often evades early diagnosis. Its hallmark clinical manifestation, hyperglycemia, is strongly associated with increased risk for myocardial infarction, stroke, microvascular complications, and mortality.1–3
The earliest symptoms of hyperglycemia may include polyuria, polydipsia, weight loss (occasionally with polyphagia), and blurred vision.4 Some patients with chronic hyperglycemia may experience impaired growth and susceptibility to certain infections.4 When diabetes is uncontrolled, acute hyperglycemia with ketoacidosis or nonketotic hyperosmolar syndrome may occur, which can be life-threatening.4
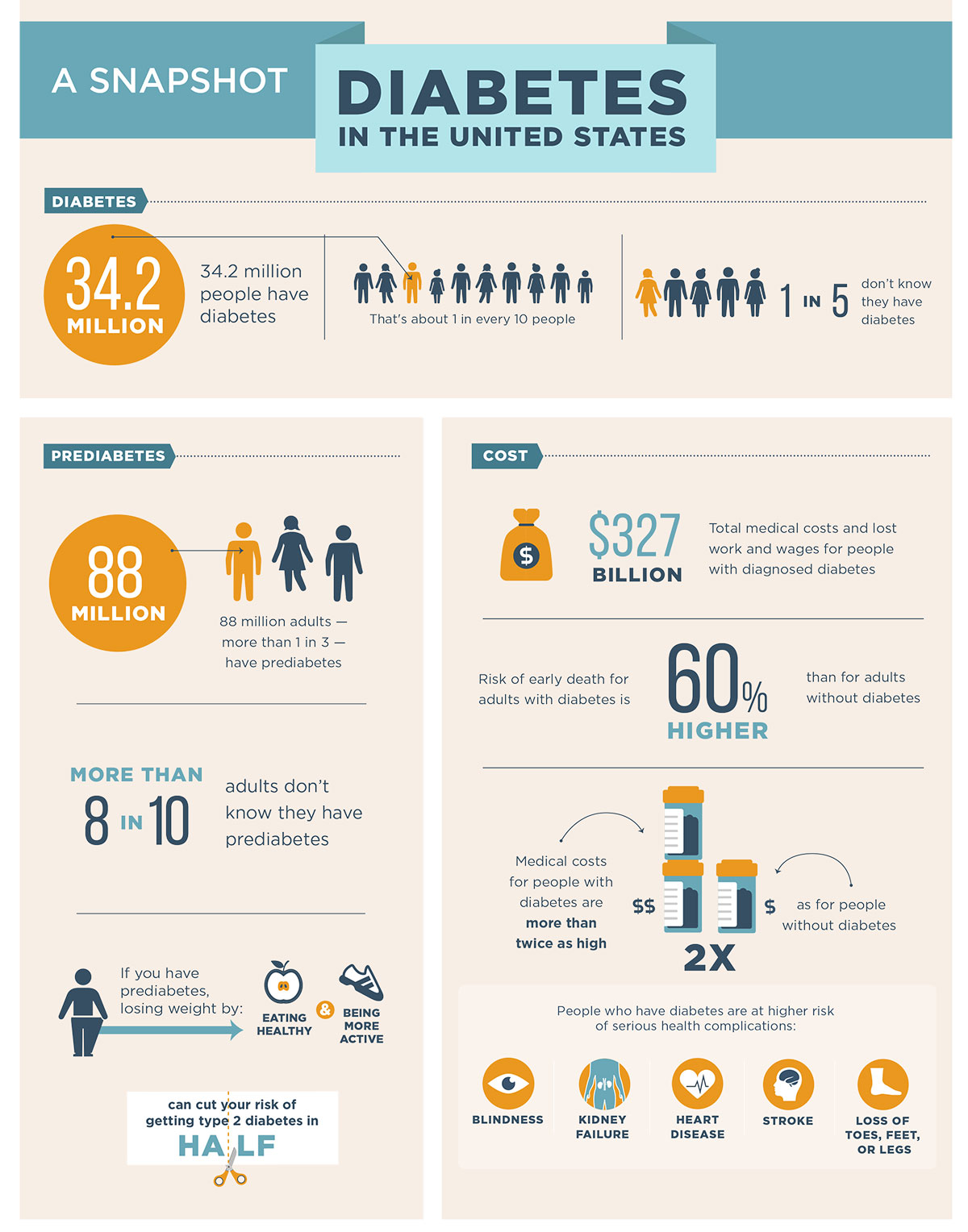
In many cases, diabetes is asymptomatic until complications manifest themselves. It is believed that type 2 diabetes remains undiagnosed in as many as 25% of people who have it.5,6 An estimated 88 million people ≥18 years old (or 34.5% of the U.S. adult population) have prediabetes, and the vast majority of those people are unaware of their condition.7,8
Early intervention: identifying patients at risk
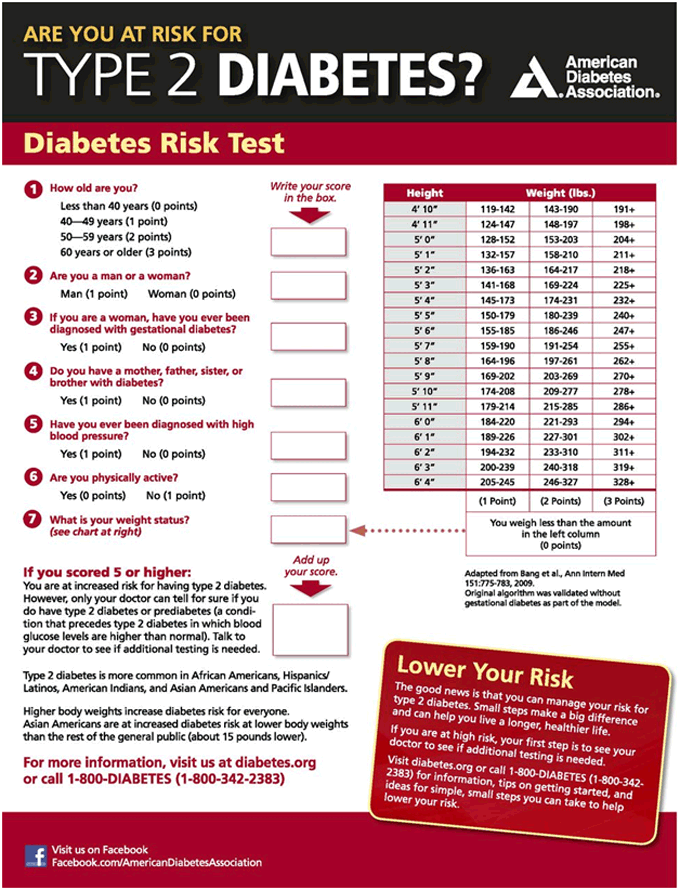
Healthcare providers have an opportunity to identify people at risk for diabetes by asking patients about symptoms and assessing for common risk factors during office visits. These common risk factors include obesity and elevated BMI, sedentary lifestyle, family history of the disease, high blood pressure, and a history of gestational diabetes. Although nonwhite minorities and people above the age of 45 years may be at increased risk, it should be noted that diabetes affects people of all ages, races, and ethnicities, and it is increasingly being seen in young adults, teenagers, and even children.7,10
Interventions that can prevent or delay the worsening of diabetes and the onset of complications can only be initiated in patients whose diabetes has been diagnosed. National guidelines for diabetes screening have been released by the Centers for Disease Control and Prevention, the American Diabetes Association, and the Preventive Services Task Force. In addition, a number of risk assessment tools has been developed to help identify patients who are in need of testing.5,11-14 The American Diabetes Association has also developed a risk test that is designed to help patients and providers quickly and easily assess diabetes risk and determine the need for diagnostic testing.5,9
Source: American Diabetes Association. Standards of Medical Care in Diabetes- 2020. Diabetes Care. 2020, (Suppl1)S14-S31.
Diagnostic Tests
A number of tests are available to diagnose diabetes and to detect prediabetes. Most often, the disease is diagnosed based on plasma glucose criteria, including A1c, fasting plasma glucose (FPG), or the 2-hour plasma glucose (2-hr PG) value after a 75 g oral glucose tolerance test (OGTT).5 Importantly, diabetes may be identified anywhere along the spectrum of clinical scenarios, including in low-risk people who happen to have glucose testing, in those whose testing is triggered by risk assessment, and in those who are symptomatic.5
The American Diabetes Association recommends that screening for prediabetes with an informal assessment of risk factors should be considered in all adults. Moreover, testing for prediabetes should be considered in adults of any age who are overweight or obese (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian Americans) and have ≥1 risk factor for diabetes, such as family history, history of gestational diabetes, and/or advanced age. Testing for diabetes should be done in all people over the age of 45 years and should be repeated a minimum of every three years when results are normal.5
Figure 1: Screening and Diagnosis of Prediabetes and Diabetes5
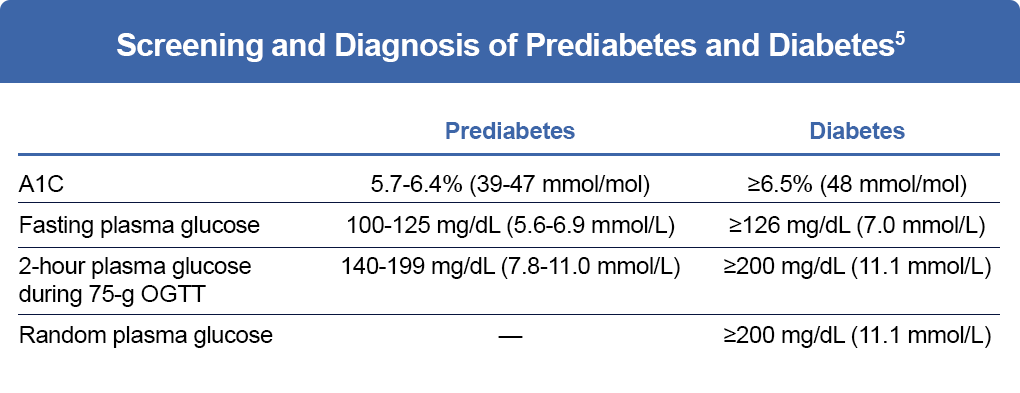
It is important that risk assessment and testing be performed regularly in clinical practice to curb the rising epidemic of diabetes and to initiate treatment in patients before the onset of advanced disease and potentially debilitating complications.5
References
- Fonseca VA. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009;32(suppl 2):S151-S156.
- Stratton IM, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405-412.
- Nichols GA, et al. Progression from newly acquired impaired fasting glucose to type 2 diabetes. Diabetes Care. 2007;30:228-233.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62-S69.
- American Diabetes Association. Standards of Medical Care in Diabetes — 2020. Diabetes Care. 2020;(suppl 1):S14-S31.
- Anderson AE, et al. Electronic health record phenotyping improves detection and screening of type 2 diabetes in the general United States population: a cross-sectional, unselected, retrospective study. J Biomed Inform. 2016;60:162-168.
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020. https://www.cdc.gov/diabetes/data/statistics/statistics-report.html.
- American Diabetes Association. Statistics about diabetes. https://www.diabetes.org/resources/statistics/statistics-about-diabetes.
- Centers for Disease Control and Prevention. Infographic: a snapshot of diabetes in America. https://www.cdc.gov/diabetes/pdfs/library/socialmedia/diabetes-infographic.pdf.
- Black SA. Diabetes, diversity, and disparity: what do we do with the evidence? Am J Public Health. 2002;92:543-548.
- CDC Diabetes Cost-Effectiveness Study Group. The cost-effectiveness of screening for type 2 diabetes. JAMA. 1998;280:1757-1763.
- US Preventive Services Task Force. Screening for type 2 diabetes mellitus in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;148:846-854.
- Bang H, Edwards AM, Bomback AS, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151;775-783.
- Heikes KE, Eddy DM, Arondekar B, Schlessinger L. Diabetes Risk Calculator: a simple tool for detecting undiagnosed diabetes and pre-diabetes. Diabetes Care. 2008;31:1040-1045.