Pregnant Women
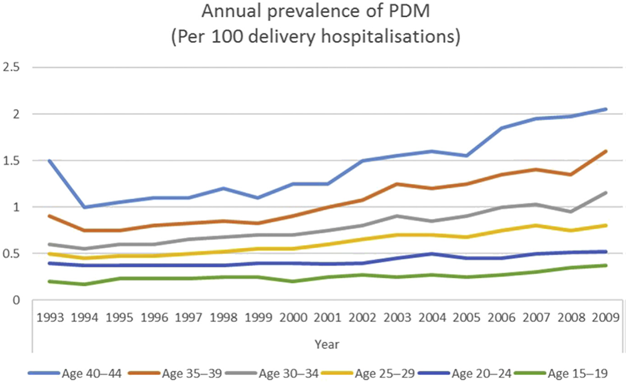
Source: Sugrue R, Zera C. Pregestational Diabetes in Pregnancy. Obstet Gynecol Clin North Am. 2018;45(2):315-331.
Adverse maternal and fetal consequences of poor glycemic control include2:
- congenital anomaly
- miscarriage
- pre-eclampsia
- preterm delivery
- macrosomia
- stillbirth
- neonatal hypoglycemia
Insulin is the preferred anti-hyperglycemic agent in pregnant women. Insulin requirements may change during pregnancy.3
|
ADA-recommended targets for women with Type 1, Type 2 or Gestational Diabetes4 |
| ○ Fasting: >95 mg/dL (5.3mmol/L) and either
• One-hour postprandial, 140 mg/dL (7.8 mmol/L) or • Two-hour postprandial, 120 mg/dL (6.7mmol/L) |
| ○ individualized A1C target of >6% (42 mmol/mol)* to >7% (53 mmol/mol)** |
| *associated with lowest rate of adverse fetal outcomes
** A1C should be used as a secondary measure of glycemic control in pregnancy, after self-monitoring of blood glucose |
Source: American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43(Supplement 1):S183-S192.
References:
- Sugrue R, Zera C. Pregestational Diabetes in Pregnancy. Obstet Gynecol Clin North Am. 2018;45(2):315-331.
- Etomi O, Banerjee A. The management of pre-existing (type 1 and type 2) diabetes mellitus in pregnancy. Medicine. 2018;46(12):731-737.
- O’Neill SM, et al. Different insulin types and regimens for pregnant women with pre-existing diabetes. Cochrane Database Syst Rev. 2017;2:CD011880.
- American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes — 2020. Diabetes Care. 2020;43(Supplement 1):S183-S192.
Resources:
American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43 (Supplement 1):S183-S192.
ACOG Practice Bulletin No. 201 Summary: Pregestational Diabetes Mellitus. Obstet Gynecol. 2018;132(6):1514-1516.